Channeling Pain Into Purpose
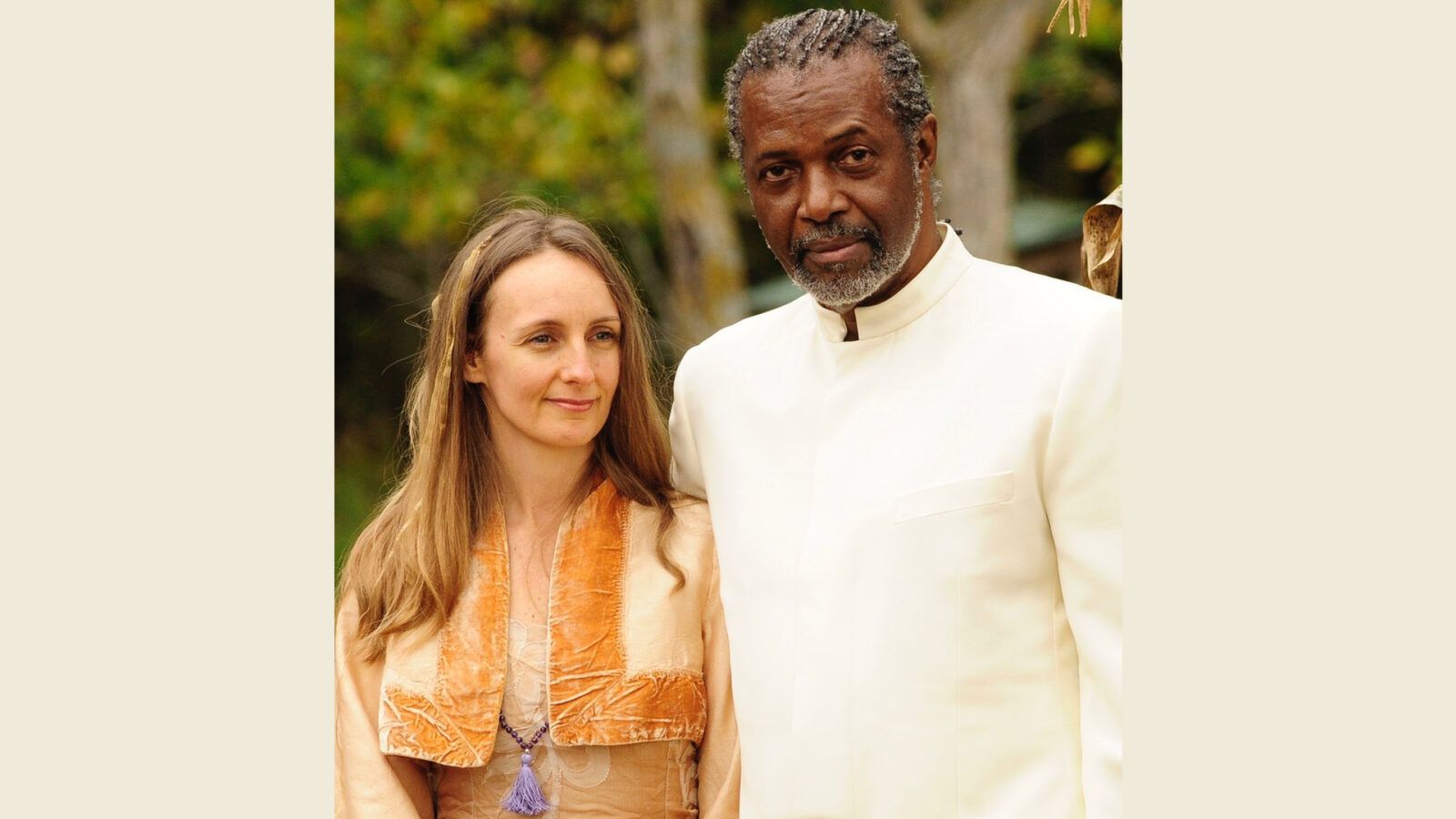
By Debbie Haine Vijayvergiya
Since I was a young girl, the only thing I was 100% certain of was that one day I would be a mom.
My first pregnancy was completely normal and resulted in a healthy picture-perfect baby girl. However, things became eventful a week later when a late presentation of Group B Strep went undiagnosed and nearly killed me. The doctor, who was covering for my Obstetrician while he was away, ignored my symptoms and concerns. I called the office repeatedly over the week; I shared with the doctor and nurses that I was in so much pain that I was consuming Percocet’s like they were tic tac’s. Even then, no one ever thought that this was alarming. Instead, they chalked it up to me being a ‘tired and hormonal new mom.’
A week to the day that I returned home with my beautiful baby girl, I arrived in the ER in complete septic shock. Thankfully, there were some truly exceptional doctors in the ER that day who saved my life. When my OB returned from vacation, he visited me in the hospital, apologizing profusely for the abysmal care I had received from his colleague. He also told me I would be dead if I stayed home another day.
My recovery was long and hampered by complications from the infection, including a blood clot resulting from the subpar PICC line courtesy of a rushing and impatient hospital staffer. My friends would often ask me if I wanted more babies after all that I had been through. I was always quick to reply, absolutely! At that point, I was convinced that I had paid my dues to the fertility gods and that nothing worse could happen to me.
The following year, I experienced my first miscarriage, which I was able to easily make peace with as I was still in recovery mode. The next year, I suffered my second miscarriage—which was a much bigger pill to swallow. After 2 weeks of bed rest, an ambulance ride, 10 hours in the ER, and compassionless care, I returned home broken. A year later I was pregnant yet again, for the fourth time in 4 years. Once I made it through my first trimester, I gave a deep sigh of relief and allowed myself to believe that everything would be ok.
Unfortunately, I wasn’t that lucky. On July 7th, 2011, my life irrevocably changed while at a routine checkup when my OB could not detect my daughter Autumn’s, heartbeat. My world came crashing down around me as I was suddenly thrust into any expectant mother’s worst nightmare. Time stopped moving for me that day— and my life has never been the same since. My doctors led me to believe that my losing Autumn was as rare as being struck by lightning. But I soon learned this wasn’t the case and that stillbirths are one of the most common adverse pregnancy outcomes, with tens of thousands of babies born still every year in this country. I learned that many of these deaths were preventable and were happening in otherwise healthy, low-risk pregnancies. Up to this point, I had always considered myself educated, yet there I was, unaware of the realities of stillbirth.
I suddenly found myself faced with the reality that this tragic maternal health issue was being seriously neglected. I never knew how risky the business of a baby having truly was. Losing Autumn was the final straw for me. After everything that I had been through, I had to act. I couldn’t sit idly by and let others suffer as we had. I was compelled to help them and found that my only path forward was to channel my pain into purpose.
And so, I set forth on my advocacy journey, sharing my story and working tirelessly for the past 11+ years to put stillbirth on the map in this country. Some of that work includes helping to develop and champion multiple pieces of legislation, such as the bipartisan Stillbirth Health Improvement and Education (SHINE) for Autumn Act, which we hope to see re-introduced into the 118th Congress, one day soon.
Advocacy was never a part of my master plan, but here I am. And while none of this work will bring Autumn back or erase the trauma I’ve experienced; it will save lives. Sadly, we will never truly know if Autumn’s death was preventable, but many of the medical errors and near misses I have endured over the years were. Far too many communication breakdowns almost cost me my life and psychologically scarred me for the rest of my days. But it didn’t have to be this way. Something must change.
Elevating parent voices is a powerful form of advocacy, whether it is for stillbirth and/or patient safety. However, the real change depends on the patient and providers’ partnership. Safe and reliable healthcare is attainable— once we start working together. To learn more about how you can create a safer and brighter future for all, go to Patients For Patient Safety US.