IN THE NEWS
Biden-Harris Administration Announces Progress and New Commitments to Improve Patient and Health Care Workforce Safety
PFPS US Latest Press Release
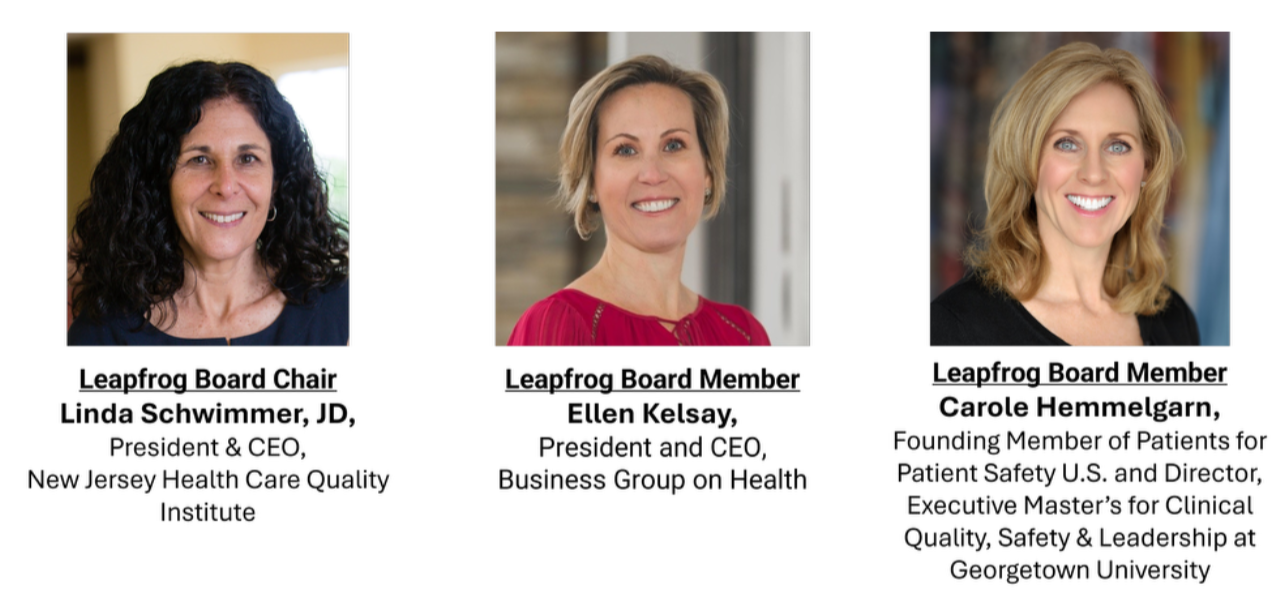
LEAPFROG ANNOUNCES THE ELECTION OF A NEW BOARD CHAIR, TWO NEW BOARD MEMBERS, AND NEW OFFICERS
Join Us for Film Screenings
“The Pitch: Patient Safety’s Next Generation”
You are invited to attend “The Pitch: Patient Safety’s Next Generation”
PFPS US invites you to attend a special screening of The Pitch: Patient Safety’s Next Generation.
From the Director of To Err Is Human: A Patient Safety Documentary (2018) comes a new documentary about the evolving role of technology in improving patient safety across medicine.
Through expert interviews, real-world technology solutions, and one young innovator’s journey into the layered business of medicine, The Pitch showcases the immense effort required to break into the healthcare industry with innovations and the importance of collaboration between those inside and outside of the medical space.
The Pitch is going on a 2024 release tour, consisting of 5 special screenings on both coasts:
Each screening will feature a panel moderated by Director and Editor Mike Eisenberg and filled with local healthcare professionals and patient safety innovators.
Can’t attend? You still have multiple options to watch “The Pitch”!
The film will be released on streaming platforms September 17th, World Patient Safety Day. You can pre-order now on iTunes and AppleTV+ (link). The film will also be available on Amazon Prime Video, VUDU, Google Play, YouTube, and Vimeo.
Dozens of screenings are also being hosted by hospitals, universities, and non-profits across the country. Check if “The Pitch” is coming to your area by visiting http://www.thepitchdocumentary.com/.
PFPS US Medicare Statement FY 2025
From NBC NEWS

A quick, cheap test could protect against fatal chemo overdose. Why do few cancer doctors use it?
Patients Safety Awareness Week
with Col. Steven L. Coffee
IHI National Patient Safety Awareness Week
Clinical Center Grand Rounds Patient Safety Week Engaging Patients as Partners
Patients hate American health care.
But presidential candidates aren't talking about it.
Karen Weintraub | USA TODAY
If only Cindy Russo had a spare $200 two years ago, she might have avoided her current nightmare.
Doctors might have caught her cancer sooner if she hadn't put off a mammogram, knowing it would lead to an ultrasound not fully covered by insurance.
And they might have found it sooner if, when she did get around to scheduling an ultrasound, an overdue bill from the last one hadn't caused further delay.
So as it was, Russo, 47, of Long Island, New York, went a few years between mammograms. When she finally got checked out ‒ when the pain finally drove her to stop putting it off ‒ there were three cancerous lumps in her breast.
Now, the single mother of two boys, 8 and 11, is even more cash-strapped.
Palooza 2024 Connected Healthcare
Patient Safety Panel

Patient Safety Proposals Reach President,
But Action Still A Question
Michael L. Millenson - Contributor

Getting the president of the United States to consider enacting your policy proposals is a major achievement. Having him actually implement them is an accomplishment that can change lives.
The patient safety movement reached that first milestone with a recent report by the President’s Council of Advisors on Science and Technology entitled, A Transformational Effort on Patient Safety. Whether advocates achieve the second, crucial goal remains very much an open question.
The PCAST casts a wide net, examining everything from nanotechnology to the public health workforce. It appears until now to have addressed patient safety only tangentially, when in 2014 it was a small part of a larger report on accelerating health system improvement through systems engineering. Many of that report’s almost decade-old recommendations – for example, “paying for volume rather than volume” and “sharing best practices” – unfortunately read as if they could have been written today.
The good news for patient safety advocates is that President Joe Biden has shown a genuine understanding of the issue. Thanks to a long-standing relationship with Joe Kiani, founder of Masimo Corp. and of the Patient Safety Movement Foundation, Biden keynoted PSMF meetings in 2015 and 2017. Kiani was appointed to the PCAST by Biden in 2021 and was co-lead, along with the chief scientific officer of Microsoft, of a special Working Group on Patient Safety that helped prepare the report.
President's Council of Advisors on Science and Technology
(PCAST)
REPORT TO THE PRESIDENT
A Transformational Effort on Patient Safety
Latest News from the
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services (CMS) have included several new or expanded provisions designed to improve patient safety and health equity in the Final Rule for Federal Year 2024, which begins on October 1, 2023. Many thanks to the PFPS US Champions who signed on to the PFPS US Public Comment that we filed as well as those who made public comments of your own. Because CMS is committed to count, read and consider every comment filed, our comments truly make a difference.
Many things we advocated for made the Final Rule, including:
- Implementation of three new electronic clinical quality measures for pressure ulcers, kidney injuries, and excessive radiation doses when doing diagnostic CT (Computed Tomagraphy) scans
- Inclusion of the Severe Sepsis and Septic Shock Early Management Bundle measure in the Hospital Value-Based Purchasing Program, which will reward hospitals financially for implementing the sepsis bundle
- Expansion of the Health Equity and Social Determinants of Health (SDOH) measures adopted last year, which PFPS US supported, from hospitals to now include public reporting by Cancer centers, with notice of plans to further expand the collection, analysis and public reporting of health equity and SDOH data in future years
- Public reporting by Long Term Care Hospitals as to whether medication lists are provided to both patient and subsequent provider upon discharge or transfer
- Recognition of Homelessness as a medical condition complication or comorbidity for which hospitals can receive additional payment for care
- New requirements that hospitals attest to annually assessing safety issues in the use of electronic health records
In addition, the Final Rule acknowledges comments made, as PFPS US did, in recognizing the importance of screening geriatric patients for at risk conditions when they are treated in Emergency Rooms or undergo elective surgeries. CMS recognizing geriatrics patients as a particularly vulnerable population is strongly indicative that our comments were heard and that these measures will be considered again next year.
More information here:
PCAST Approves Patient Safety Recommendations.
Publication of the full report expected in September
On July 28th, the President’s Council of Advisors on Science and Technology (PCAST) approved several patient safety recommendations to be included in an Executive Order that will go to President Biden. The report was developed by a PCAST Patient Safety Work Group that has been meeting since last year. The recommendations include prioritizing patient safety as a national public health priority with strong federal leadership, including a National Patient Safety Coordinator that reports to the President. Other recommendations address transparency, health equity, patient and family engagement, expanding research to better identify risks of harm, accountability and ensuring a culture of safety.
Sue Sheridan, Founding Member of Patients for Patient Safety, (PFPS US), was on the Patient Safety Working Group. We are pleased to see many PFPS US priorities embedded in these new recommendations. The report is due to be published in September. Below is the recording of the public meeting where the Working Group’s high level recommendations were presented and approved, as well as the slide deck for you to download.
CNN Health: A national safety board made transportation safer and could do the same for health care, advocates say
By Mary Chris Jaklevic, KFF Health News
Published 6:10 AM EDT, Tuesday, May 30, 2023
KFF Health News —
People concerned about the safety of patients often compare health care to aviation. Why, they ask, can’t hospitals learn from medical errors the way airlines learn from plane crashes?
That’s the rationale behind calls to create a “National Patient Safety Board,” an independent federal agency that would be loosely modeled after the National Transportation Safety Board, which is credited with increasing the safety of skies, railways, and highways by investigating why accidents occur and recommending steps to avoid future mishaps.
But as worker shortages strain the U.S. health care system, heightening concerns about unsafe care, one proposal to create such a board has some patient safety advocates fearing that it wouldn’t provide the transparency and accountability they believe is necessary to drive improvement. One major reason: the power of the hospital industry.
Two measures are underway to create a safety board: A bill filed in the U.S. House in December by U.S. Rep. Nanette Diaz Barragán (D-Calif.), which is expected to be refiled this session, calls for the creation of a board to help federal agencies monitor safety events, identify conditions under which problems occur, and suggest preventive measures.
Who Killed Patient Safety
The medical community’s commitment to patient safety has withered over the past 10–15 years after the original call to action in 2000 with the release of the IOM report, To Err is Human.
The tragedy of this decline in action around safety lies in the lives of the families like ours, who have lost loved ones, been harmed, and often permanently injured by medical error.
What was once a motivating call to action, safety in hospitals and oversight by our government has been deprioritized, defunded, and devalued leaving patients like us to wonder: What happened to Patient Safety.
PFPS US OIG Complaint
Date Filed: May 12, 2022
PFPS US Founding Members submitted a complaint and request for investigation on May 12th to the HHS Office of Inspector General (OIG) regarding Vanderbilt University Medical Center, the Tennessee Department of Health and CMS related to case 2019-A-76, State of Tennessee vs Radonda Vaught. We chose to go forward with this because, to our knowledge, nobody else has asked for an investigation into the legal and ethical duties of organizational leaders at Vanderbilt, the Tennessee Department of Health and at CMS.
We based this complaint on what we know from the CMS investigation and the testimony during the trial. We are aware that there could be information of which we are unaware, but feel that if there is more to know, then it should be shared with a very concerned public that fears that obscuring the truth about harm from medical errors is an accepted way of doing business.
We also acknowledge that nothing may come of this complaint, but if that is the case, we will have a better understanding of the limitations of our healthcare oversight bodies and will support a national call for an authoritative oversight body that holds healthcare system and state leadership accountable to the public.
CMS: Vanderbilt Report
An unannounced onsite survey was conducted 10/31/18 to 11/8/18 to investigate complaint # TN00045852.
An entrance conference was held with the Regulatory Officer, Accreditation Specialist and the Senior Quality and Patient Advisor. They were informed of the nature of the complaint.
A telephone exit conference was held on 11/8/18 at 2:00 PM. The Regulatory Officer, Accreditation Specialist and the Senior Quality and Patient Advisor, and the Accreditation Regulatory Specialist were notified of Immediate Jeopardy in the areas of 482.13 Patient Rights, 482.23 Nursing Services. They were afforded the opportunity to ask questions of the survey team.

